Anonymous, MD,1 Sucharit Bhakdi, MD, and Michael Palmer, MD
Abstract: Many countries are currently experiencing a wave of COVID-19 “breakthrough cases” in spite of high vaccination rates. In this paper, we explain the fundamental reason why such cases had to be expected: the antibodies induced by intramuscular vaccination will only circulate in the bloodstream, but they will not reach the surface of the mucous membranes in the upper airways. We also briefly discuss possible mechanisms of vaccine-induced immunopathology.2
Some of material discussed in this paper is also covered in a recent video by Dr. Bhakdi.
1. Introduction: All antibodies are not created equal
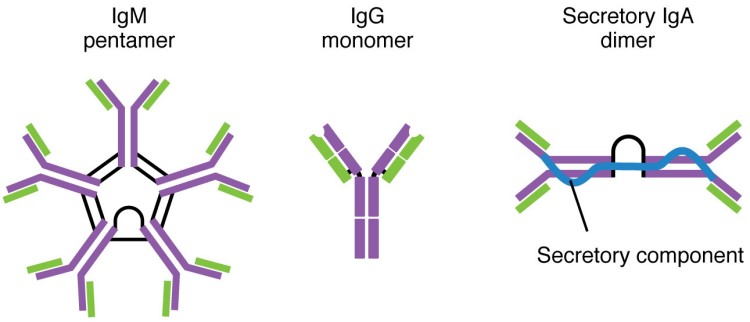
There are different types of antibodies utilized by the human immune system. The major ones are IgM, IgG and IgA [1]; there are two other classes, IgD and IgE, but there is no need to discuss them here.
IgM is generated in the early stages of an adaptive immune response and is then gradually replaced with IgG antibodies. Both IgM and IgG circulate mainly in the bloodstream. IgG is the most abundant antibody in the blood. On the other hand, while some IgA is found in the bloodstream as well, most IgA is secreted across the mucous membranes of the respiratory tract and the gut, which it then covers and protects.
When our immune system is confronted with an invading pathogenic microbe, the predominant type of antibody it produces depends on the location of that pathogen. If the pathogen is encountered in the bloodstream or inside of tissues within the body, e.g. the muscle, then the immune system will produce mainly IgG antibodies, which will accumulate in the bloodstream. On the other hand, if the pathogen is introduced through the respiratory tract (e.g. the nostrils), then the immune system will produce mainly IgA antibodies—to be more specific, secretory IgA, or sIgA.
While sIgA dominates in the upper airways, some IgG is found along with IgA in the lower airways, that is, the bronchi and lung alveoli. In addition to sIgA, an immune response triggered by a respiratory tract infection will also generate both IgG and IgA within the bloodstream, which provides a safeguard in case the barriers of the respiratory tract are breached and the pathogens enter the tissues. In short, sIgA is the main antibody the immune system relies on in the upper respiratory tract (URT), and it forms the first line of defense against respiratory pathogens.
2. Why is sIgA antibody important?
The key reason why an sIgA-based antibody response is desired against respiratory pathogens is that sIgA does not promote inflammation. Binding of sIgA antibodies to the antigens (such as viruses or bacteria) leads to “quiet” expulsion of these pathogens from the body, but it does not elicit any additional damaging immune responses. In contrast, an IgG-based response is followed by an inflammatory immune reaction. This reaction is triggered by a change in the molecular shape of the Fc region (the tail end) of IgG antibodies, which causes them to activate inflammatory cells as well as the serum complement system.
Since our respiratory tract constantly encounters viruses and bacteria within the air we inhale, IgA-based immune responses help avoid unnecessary and repeated inflammations in our airways. sIgA in the mucous membranes of the respiratory tract can subdue the infection and stop the transmission of these germs safely.
Considering these well-established scientific facts, it is beyond perplexing that people only talk about antibodies (mainly IgG antibodies) in the bloodstream after COVID vaccination. If a vaccine should protect us from respiratory viruses and from transmitting them to others, it should elicit an IgA-based immunity in our respiratory tract, especially in the upper airways.
3. What is really damaging our body: viruses, or our own immune system?
Respiratory viruses rarely cause direct damage to our body. It is typically the overreaction of our immune system against those viruses that does the damage [2,3]. With respect to COVID-19, a recent paper on the causation of clinically severe disease sums it up as follows [4]:
[Severity of COVID-19] is suggested not to be a direct effect of viral infection but instead to be caused by the over-activation of the immune system in response to infection, because worsening of disease coincides with the activation of adaptive immunity. This excessive immune response is frequently described as a “cytokine storm” … Together, high pro-inflammatory cytokines, known to induce collateral damage to tissues, and muted anti-viral responses suggest that an unfavorable immune response may be driving disease in patients with severe cases of COVID-19.
4. The route of vaccination matters
A vaccine that is given by intramuscular (IM) injection will mainly induce IgG antibodies in the blood; this matches the body’s response to pathogens introduced by the same route. It is well known that IM vaccines generate very little or no sIgA in the respiratory tract. Therefore, IM injection is not an efficient way of prepping our immune system against respiratory viruses. Should a full-blown pneumonia develop, circulating IgG antibodies will seep out of the capillaries into the alveoli and there help with viral clearance; therefore, conceivably an IM injection might afford some measure of protection against severe disease. On the other hand, vaccine-induced IgG antibodies may also cause exacerbate the disease (see next section). In any case, prior to inflammation, practically no IgG will be present on the respiratory mucous membranes, which leaves them vulnerable to infection. This is why the current COVID-19 vaccines cannot prevent infection or transmission of the virus [5,6]. Below is a direct quote from the review paper by McGhee et al. [6]:
It is surprising that despite our current level of understanding of the common mucosal immune system, almost all current vaccines are given to humans by the parenteral route. Systemic immunization is essentially ineffective for induction of mucosal immune responses. Since the majority of infectious microorganisms are encountered through mucosal surface areas, it is logical to consider the induction of protective antibodies and T cell responses in mucosal tissues.
Note that this statement was made already three decades ago—yet nothing has changed, and the same flawed, outdated approach of intramuscular injection has been adopted yet again with the “modern” and “high-tech” COVID-19 vaccines.
We can conclude that either the natural infection through our respiratory tract or nasal vaccination is required to induce effective immunity against respiratory viruses. With COVID-19, this is borne out by a recent animal study [7], which confirmed that the AstraZeneca COVID vaccine administered by the intramuscular route failed to protect hamsters from the infection by SARS-COV-2 or to prevent the transmission of this virus. When the vaccinated animals were challenged with the virus through the airways, they still became infected, and their lungs were damaged. On the other hand, the animals that were vaccinated by the nasal route were able to clear the viruses in the URT and prevent the infection in the lower respiratory tract (LRT).
The lack of protection against infection of the airways by serum IgG is not limited to SARS-CoV-2 and COVID. As early as 1984, Liew et al. demonstrated that the IgG found in the bloodstream is quite irrelevant for the protection against influenza virus; it is the sIgA on the mucous membranes that prevents the virus from establishing infection.
In conclusion, sIgA on the mucous membranes, especially in the URT, is necessary for effective and protective immunity against respiratory viruses, and it is induced only when the antigen is introduced via the natural route—into the URT itself. This rule applies to both natural pathogens and vaccines.
5. An IgG response can be a bad thing
Not only does IgG circulating in the bloodstream fail to prevent infection with respiratory viruses, but an IgG-based immune response can even elicit harmful inflammatory responses, causing serious tissue damage within the respiratory tract. In their recent review article on mucosal immunity to COVID-19, Russell et al. state [8]:
Most attention has been given to virus-neutralizing antibodies, especially circulating antibodies. However, these can only be effective in the prevention of infection or disease if [the antibodies] reach the mucosal surfaces where the virus is present, and it should be noted that circulating IgA, even in polymeric form, is not effectively transported into secretions. While plasma-derived IgG occurs in the URT and especially the lower respiratory tract (LRT), IgG is inflammatory in its mode of action, by the induction of such effector mechanisms as complement activation and the engagement of phagocytes such as macrophages and neutrophils as well as natural killer (NK) cells. The serious pathology of COVID-19 occurs in the terminal airways of the lungs, where circulating IgG is the dominant immunoglobulin. The resulting intense inflammation involves multiple molecular and cellular factors, including cells recruited by virus-induced chemo-attractants. ... In practical terms this means that intranasal immunization should be an effective means of generating predominantly sIgA antibody responses in the URT and LRT, where SARS-CoV-2 could be neutralized and eliminated without inflammatory consequences. In addition, it implies that assaying IgA antibodies in nasal secretions or saliva should be a more informative way of assessing effective immune responses against SARS-CoV-2, whether induced by the natural infection or by intranasal immunization. Assaying serum IgA antibodies, while of additional interest, is not a substitute, because serum IgA comes from a different source (mainly the bone marrow) and consists mostly of monomeric IgA1. This is distinct from mucosal sIgA, which … is locally synthesized by pIgA-secreting plasma cells resident in the subepithelial spaces (lamina propria) of mucosal tissues and glands … Moreover, sIgA is essentially non-inflammatory, even anti-inflammatory, in its mode of action. IgA does not activate complement …
An association of excessive IgG-based immune responses with negative clinical outcomes has also been observed after natural infection with SARS [9] and COVID-19 [4,10]. IgG antibodies will bind to virus particles first and then, via their Fc moieties (see Section 2), to Fc receptors on immune cells. The virus may then enter those cells and subsequently replicate within them. This disease mechanism is known as antibody-dependent enhancement and also occurs with other virus families [11].
In addition to aggravating acute lung disease such as in SARS and COVID-19, high concentrations of IgG are also associated with chronic inflammatory lung diseases such as idiopathic pulmonary fibrosis and chronic hypertensive pneumonitis [12]. In summary, too little IgG is a bad thing, but too much IgG is equally a bad thing.
6. Vaccination and M1/M2 macrophages
Macrophages are an important type of innate immune cells; their role is to ingest and destroy pathogenic microbes. Macrophages can adopt either an M1 or M2 type, depending on the inflammatory state of the tissue. M1 macrophages promote inflammation, whereas M2 macrophages promote wound-healing. Thus, the balance between M1 and M2 macrophages is essential for a healthy immune system.
A recent study in monkeys has demonstrated that the intramuscular injection of a vaccine against SARS-COV—the original SARS virus from 2003, which is highly homologous to the causative agent of COVID (SARS-CoV-2)—promoted the elimination of virus particles that were injected directly into the trachea, but also caused severe inflammatory injuries in the lung tissues. Inflammation was exacerbated by a shift of macrophage polarization from wound-healing M2 toward inflammatory M1 macrophages [13]. Priming the lung macrophages into M1 type leads to dangerous inflammatory diseases and tissue damages, and that’s what the IM vaccination does according to this paper.
7. Vaccination and Th2-type immunopathology
T helper cells are a type of lymphocytes that plays a key role in the stimulation and regulation of immune responses. Again, there are two major subsets of this cell type, referred to as Th1 and Th2, respectively. Th1 cells activate immune responses against intracellular pathogens, including protozoa, bacteria, and viruses. Th2 cells, on the other hand, help mount a defense against infections with worm parasites, but they also promote allergic diseases such as asthma, atopic dermatitis, and hay fever [14]. A hallmark of Th2-activated responses is an increased abundance in blood and tissues of eosinophil granulocytes. These effector cells are useful for combating worm parasites, but for little else; in allergic disease, they merely contribute to the tissue damage.
It is therefore significant that several experimental vaccines against the original SARS virus, while inhibiting proliferation of the virus within the lungs to some degree, caused Th2-type lung pathology, characterized by increased numbers of eosinophil granulocytes within and aggravated injury to the lungs [15–17]. These results indicate that the experimental vaccines against SARS-CoV may cause more severe illnesses when the vaccinated person is challenged with the real virus.
We must stress again that SARS-CoV and SARS-CoV-2 are highly homologous, which means that any risk or problem known with SARS-CoV must be considered with SARS-CoV-2 also. While the manufacturers Pfizer, Moderna, and Johnson & Johnson claim that their vaccines preferentially induce Th1 responses, supporting data from human vaccinees are scarce or lacking altogether [18–20].
8. Conclusion
All of the currently used COVID vaccines are applied by intramuscular injection, and they are therefore unable to prevent infection of the upper airways with the SARS-CoV-2 virus. In fact, in their clinical trials, none of the manufacturers even attempted to demonstrate efficacy against infection or transmission in their clinical trials [18–21], and the total lack of efficacy in the real world has since been documented in a large study published by the CDC [22]. The vaccines can, however, lead to severe respiratory immune disease, including Th2-type immunopathology and autoimmunity. When factoring in the large number of adverse events that are being reported with the current vaccines and the low case fatality rate of COVID-19, which we have discussed elsewhere [23], it is clearly more scientific and more reasonable to strive for herd immunity by natural infection rather than vaccination.
Notes
- The first draft of this document was written by a colleague who prefers to remain anonymous.
- In this updated version, a misleading statement in Section 4, pertaining to the location of IgG in the airways, has been amended.
References
- Anonymous, (2021) Antibody (Wikipedia).
- Newton, A.H. et al. (2016) The host immune response in respiratory virus infection: balancing virus clearance and immunopathology. Semin. Immunopathol. 38:471-482
- Tay, M.Z. et al. (2020) The trinity of COVID-19: immunity, inflammation and intervention. Nat. Rev. Immunol. 20:363-374
- Hoepel, W. et al. (2021) High titers and low fucosylation of early human anti-SARS-CoV-2 IgG promote inflammation by alveolar macrophages. Sci. Transl. Med. 13 (preprint)
- Kurono, Y. (2021) The mucosal immune system of the upper respiratory tract and recent progress in mucosal vaccines. Auris, nasus, larynx (preprint)
- McGhee, J.R. et al. (1992) The mucosal immune system: from fundamental concepts to vaccine development. Vaccine 10:75-88
- van Doremalen, N. et al. (2021) Intranasal ChAdOx1 nCoV-19/AZD1222 vaccination reduces viral shedding after SARS-CoV-2 D614G challenge in preclinical models. Sci. Transl. Med. 13 (preprint)
- Russell, M.W. et al. (2020) Mucosal Immunity in COVID-19: A Neglected but Critical Aspect of SARS-CoV-2 Infection. Front. Immunol. 11 (preprint)
- Lee, N. et al. (2006) Anti-SARS-CoV IgG response in relation to disease severity of severe acute respiratory syndrome. J Clin Virol 35:179-184
- Tan, W. et al. (2020) Viral Kinetics and Antibody Responses in Patients with COVID-19. medRxiv (preprint)
- Ulrich, H. et al. (2020) Dengue Fever, COVID-19 (SARS-CoV-2), and Antibody-Dependent Enhancement (ADE): A Perspective. Cytometry A 97:662-667
- Reynolds, H.Y. et al. (1977) Analysis of cellular and protein content of broncho-alveolar lavage fluid from patients with idiopathic pulmonary fibrosis and chronic hypersensitivity pneumonitis. J. Clin. Invest. 59:165-175
- Liu, L. et al. (2019) Anti-spike IgG causes severe acute lung injury by skewing macrophage responses during acute SARS-CoV infection. JCI insight 4 (preprint)
- Butcher, M.J. and Zhu, J. (2021) Recent advances in understanding the Th1/Th2 effector choice. Faculty reviews 10:30
- Bolles, M. et al. (2011) A double-inactivated severe acute respiratory syndrome coronavirus vaccine provides incomplete protection in mice and induces increased eosinophilic proinflammatory pulmonary response upon challenge. J. Virol. 85:12201-15
- Tseng, C. et al. (2012) Immunization with SARS coronavirus vaccines leads to pulmonary immunopathology on challenge with the SARS virus. PLoS One 7:e35421
- Iwata-Yoshikawa, N. et al. (2014) Effects of Toll-like receptor stimulation on eosinophilic infiltration in lungs of BALB/c mice immunized with UV-inactivated severe acute respiratory syndrome-related coronavirus vaccine. J. Virol. 88:8597-614
- Anonymous, (2021) EMA Assessment report: COVID-19 Vaccine Janssen.
- Anonymous, (2021) EMA Assessment report: COVID-19 Vaccine Moderna.
- Anonymous, (2021) EMA Assessment report: Comirnaty.
- Anonymous, (2021) EMA assessment report: COVID-19 Vaccine AstraZeneca.
- Brown, C.M. et al. (2021) Outbreak of SARS-CoV-2 Infections, Including COVID-19 Vaccine Breakthrough Infections, Associated with Large Public Gatherings—Barnstable County, Massachusetts, July 2021. MMWR. Morbidity and mortality weekly report 70:1059-1062
- Palmer, M. and Bhakdi, S. (2021) Expert statement regarding the use of Moderna COVID-19-mRNA-Vaccine in children.