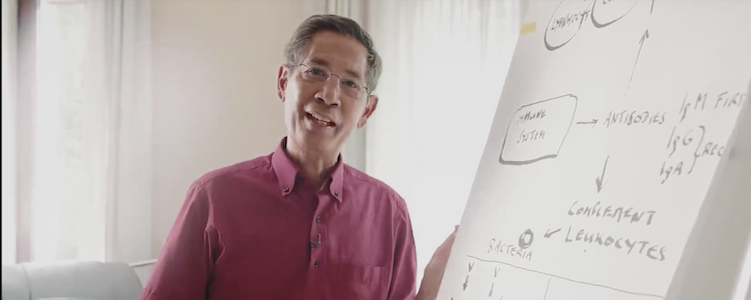
Michael Palmer, MD and Sucharit Bhakdi, MD
Some time ago, Dr. Bhakdi published a video presentation [1] which explained that cross-immunity to SARS-CoV-2 is widespread in the population, and that general vaccination is therefore not necessary or appropriate. This was disputed by Dr. Geert vanden Bossche [2]. Here, we rebut Dr. vanden Bossche’s assertions.
In the following, quotes from van den Bossche’s piece are typeset in italics, and our replies are printed in upright font shape.
1. Cross-immunity to SARS-CoV-2 exists and is cross-protective
Dr. Bhakdi is confusing all along cross-reactivity (which basically means that antibodies (Abs) or T cells induced by one CoV can BIND similar [conserved] epitopes on some other CoVs) and cross-protection. None of the publications Dr. Bhakdi is referring to has analyzed or claims cross-PROTECTION elicited by other CoVs.
Cross-protection is supported by the available evidence:
- A correlation between cross-protection and cross-reactive antibodies has been explicitly confirmed in several other studies [3–6].
- COVID-19 is more severe in younger children than in older children and adolescents [7]. This is consistent with greater protection of the latter by cross-immunity conferred by past infection with other coronaviruses.
- The low disease severity and very low case fatality rates of COVID in the general population further support protection by cross-immunity.
2. Neutralizing activity of SARS-CoV-2 antibodies
Again, Abs that bind to Sars-CoV-2 do not necessarily neutralize the virus and prevent it from entering the cell.
Apart from the fact that Dr. vanden Bossche erringly equates virus neutralization in laboratory experiments with protection from infection, his above statement applies to all viruses. Each natural virus infection will produce a multitude of clonal antibodies (“idiotypes”). At least some idiotypes will be non-neutralizing; however, other idiotypes typically will neutralize. Moreover, this is true regardless of whether these antibodies are cross-reactive or not. The argument is irrelevant.
3. Not all respiratory coronavirus induce cross-reactive antibodies effectively
In addition, Sars-CoV-2-induced Abs were only found to cross-react with 2 out of the 4 common cold CoVs (i.e., only for beta coronavirus HKU1 and OC43) and the cross-reactivity was ‘much lower than that observed for the remaining CoV epitopes.’
This is correct. However, whether it comes from some or from all coronaviruses is immaterial to the existence of cross-immunity as such. The study by Nielsen et al. [8] unambiguously demonstrated cross-immunity in almost all test persons who had been infected with SARS-CoV-2.
4. Those ghastly variants
Furthermore, his statement that people who have built immunity against CoV are automatically protected against all Sars-CoV-2 variants is not true either for exactly the same reasons (i.e., Abs that bind to variants do not necessarily neutralize them and could even be at risk of causing Ab-dependent enhancement of disease; ADE).
Dr. vanden Bossche contends that immunity to CoV rests on the presence of neutralizing antibodies that will fail their duty when variants arise. This assumption lacks a scientific basis. It is common knowledge that protection against severe respiratory viral disease derives primarily from cellular immunity. Reactive lymphocytes limit viral multiplication at sites of infection. Antibodies merely play supportive roles in preventing viral spread in the bloodstream.
“Variants” (mutant strains) will arise due to “antigenic drift” with any RNA virus that propagates within the human population, and SARS-CoV-2 is no exception. Antigenic drift occurs in minuscule steps and, as is well known, the genetic and antigenic differences between the original (Wuhan) strain of SARS-CoV-2 and any of its variants are vanishingly small relative to the difference between any SARS-CoV-2 strain and the respiratory coronavirus that confer cross-immunity. That such minuscule changes should substantially affect immunity and even promote ADE is not credible.
Cross-reactive T-cell immunity, which is a pillar of immunological competence against respiratory viruses, has been documented with respect to SARS-CoV-2 since 2020 [9,10]. Antibody response and T cell response are correlated; thus, fixating on the properties of antibody idiotypes only when trying to gauge overall immunity misses the mark.
5. Are the asymptomatically infected doomed?
Vanden Bossche insists that the study by Nielsen et al. [8] “does not truly provide information on asymptomatically infected individuals” but that the people referred to in the study must instead have had mild symptoms, and further that “asymptomatically infected individuals do not develop long-lived or mature anti-S [anti-spike] Abs and have not been reported to develop memory B cells or CYTOTOXIC memory T cells. Consequently, previously asymptomatically infected people (i.e., the majority of the population) cannot rely on ACQUIRED immunity for protection against infection or disease.”
Unlike vanden Bossche, we are not concerned about the difference between mild symptoms and none at all; quite obviously, both groups of patients were protected from severe disease. More interesting than this quibble is his parenthetical assertion that the majority of the population has already been “asymptomatically infected” with COVID. He further assumes that such individuals do not develop any immunological memory. Several questions then arise:
- How was it established that the majority of the population had already experienced asymptomatic infection? Positive PCR tests alone cannot be accepted as proof of this assertion.
- If any individuals were indeed asymptomatically infected, then what, if not cross-immunity, prevented their infection from becoming clinically manifest?
- If these individuals were protected from manifest disease during their first infection, why should we assume that they will fare any worse when infected again? We hope that vanden Bossche will resist the temptation to trot out the fearsome Delta variant in response.
6. Of people and of test tubes
In the Danish study [Nielsen et al.] at least nine individuals were unable to fully neutralize viral infection
Neutralization is a function of antibodies or serum samples, not of individuals. Clinical immunity may exist even without neutralizing antibodies. Moreover, neutralization was determined using a recombinant pseudo-virus that expressed the SARS-CoV-2 spike protein, but none of the other SARS-CoV-2 proteins. It cannot simply be assumed that none of these could contribute to neutralization.
In addition, it is stated in the discussion [again Nielsen et al.] that ‘some rare individuals have no detectable immunological memory to Sars-CoV-2.’
These “rare individuals” were most likely those with low cross-immunity and false-positive PCR tests. The fact that a lack of immunological memory is rare supports rather than contradicts the prevalence of cross-immunity.
To my knowledge, there is no evidence that Sars-CoV-2-induced CD8+ T cells provide cross-protection from common cold viruses or vice versa and this wasn’t even part of this investigation.
Cross-protection from common cold viruses by immunity to SARS-CoV-2 is not the point. We are only discussing cross-immunity in the opposite direction, which has indeed been detected [9,10] and most likely contributes to the clinically manifest cross-protection.
7. On herd immunity
So, with all my respect for Dr. Bhakdi, the conclusion that herd immunity would already be established and would simply need to be recalled upon exposure to SARS-CoV-2 is not correct. By the way, if this were true, we would not currently be witnessing a fulminant propagation of the delta variant in several countries.
Herd immunity in the strict sense—namely, a high prevalence of sterilizing immunity that prevents a virus from effectively propagating within the population—is problematic with any respiratory virus. Dr. Bhakdi was using the term loosely, referring widespread immunity that is sufficient to protect from severe disease. The pervasiveness of such immunological protection is indeed apparent from the very low rates of fatality or severe disease in the general population, and particularly among those without co-morbidities. However, we agree with vanden Bossche that it would have been better to use the term “widespread protective immunity” rather than “herd immunity” in this case.
8. Summary
With the exception of the above single point of terminology, we see no merit in Dr. vanden Bossche’s response. We maintain that Dr. Bhakdi’s interpretation of the studies he highlighted in his video presentation are fully supported by the available scientific literature.
References
1. Bhakdi, S. (2021) Proof that puts an end to the SARS-CoV-2 narrative.
2. Vanden Bossche, G. (2021) Response to Dr. Bhakdi.
3. Dugas, M. et al. (2021) Less severe course of COVID-19 is associated with elevated levels of antibodies against seasonal human coronaviruses OC43 and HKU1 (HCoV OC43, HCoV HKU1). Int J Infect Dis 105:304-306
4. Dugas, M. et al. (2021) Lack of antibodies against seasonal coronavirus OC43 nucleocapsid protein identifies patients at risk of critical COVID-19. J Clin Virol 139:104847
5. Yamaguchi, T. et al. (2021) Immunity against seasonal human coronavirus OC43 mitigates fatal deterioration of COVID-19. Int J Infect Dis (preprint)
6. Yaqinuddin, A. (2020) Cross-immunity between respiratory coronaviruses may limit COVID-19 fatalities. Med. Hypotheses 144:110049
7. Tsabouri, S. et al. (2021) Risk Factors for Severity in Children with Coronavirus Disease 2019: A Comprehensive Literature Review. Pediatric clinics of North America 68:321-338
8. Nielsen, S.S. et al. (2021) SARS-CoV-2 elicits robust adaptive immune responses regardless of disease severity. EBioMedicine 68:103410
9. Le Bert, N. et al. (2020) SARS-CoV-2-specific T cell immunity in cases of COVID-19 and SARS, and uninfected controls. Nature 584:457-462
10. Grifoni, A. et al. (2020) Targets of T Cell Responses to SARS-CoV-2 Coronavirus in Humans with COVID-19 Disease and Unexposed Individuals. Cell 181:1489-1501.e15